Daily Mood Diary (DMD): a proposal for tracking change in subjective mood
Saxby Pridmore1, Yvonne Turnier-Shea2, Renee Morey2, Matthew Fasnacht3 and William Pridmore4
1University of Tasmania, Hobart, Australia; 2Saint Helens Private Hospital, Hobart, Australia; 3Older Persons Mental Health Services, Tasmania, Australia; 4Mental Health Services, Tasmania, Australia.
Correspondence: Prof Saxby Pridmore: s.pridmore@utas.edu.au
Received: 13/2/2022; Accepted: 19/2/2022
Keywords: Major depressive disorder; psychometrics; subjective mood.
[citation: Pridmore, Saxby;Turnier-Shea, Yvonne; Morey, Renee; Fasnacht, Matthew; Pridmore, William (2022). Daily Mood Diary – a proposal for tracking change in subjective mood. DHH, 9(1):http://www.journalofhealth.co.nz/?page_id=2691].
Abstract
The quantification of subjective mood is an important part of the assessment of mood. We describe the Daily Mood Diary (DMD) which is in restricted clinical use and undergoing further consideration. It is based on the standard ubiquitous health question, “How do you feel today”. It is unique in that it provides a progressive daily total – this introduces its weakness, that it must be applied every day – any lapse in daily collection introduces error. A copy of the score sheet is provided and evaluation is encouraged.
Description
The Daily Mood Diary (DMD) is a tool designed to provide a fine-grained picture of change in subjective mood over time. It is currently used in clinical practice at the Saint Helen’s Private Hospital, Hobart, Australia.
A standard method of tracking change in mood is to compare the scores of a quantitative test (such as the Hamilton Depression Rating Scale) administered at two points in time. That method is valuable but does not give early information or evidence of variations in the rate of change during the period of investigation.
The DMD is fundamentally the attachment of numbers to the ubiquitous doctor-to-patient question: “Compared to yesterday, how do you feel today?” It can be administered by staff as a verbal question with responses entered in the clinical notes or self-administered and recorded by the patient.
There are 3 optional responses to this question: ‘The same’; ‘Better’; ‘Worse’. If the individual answers, either ‘Better’ or ‘Worse’, they are asked to evaluate, “By how much?” Again, there are three response options: ‘A tiny bit’; ‘Quit a bit’; ‘A lot’.
‘Better’ is given a plus sign, and ‘Worse’ a minus sign. ‘A tiny bit’, ‘Quite a bit’, and ‘A lot’ are given the numerical values, 1, 2, and 3. The arithmetic total can be calculated for a known period. This allows the comparison of responses of separate individuals to the same treatment, or of the same individual to different treatments.
Also, the patient response can be graphed – this allows changes in slope (rate of change) to be visually identified. Treatments of depression may take weeks to produce an effect – the DMD can indicate when/if change begins.
Because patients are being asked to compare the day they are currently living with the previous day, it is better if the question is asked after a good part of the day has been experienced, at about evening mealtime, or later.
When drawing a graph, response to the first day of treatment is placed at 1 on the x-axis (Time/days) – that is, the numbers on the x-axis represent completed days. The y-axis indicates progressive response.
The DMD needs to be administered every day – missing a day introduces an error. This can be a major problem and the tool can only be recommended when adequate administration of the test is available and committed.
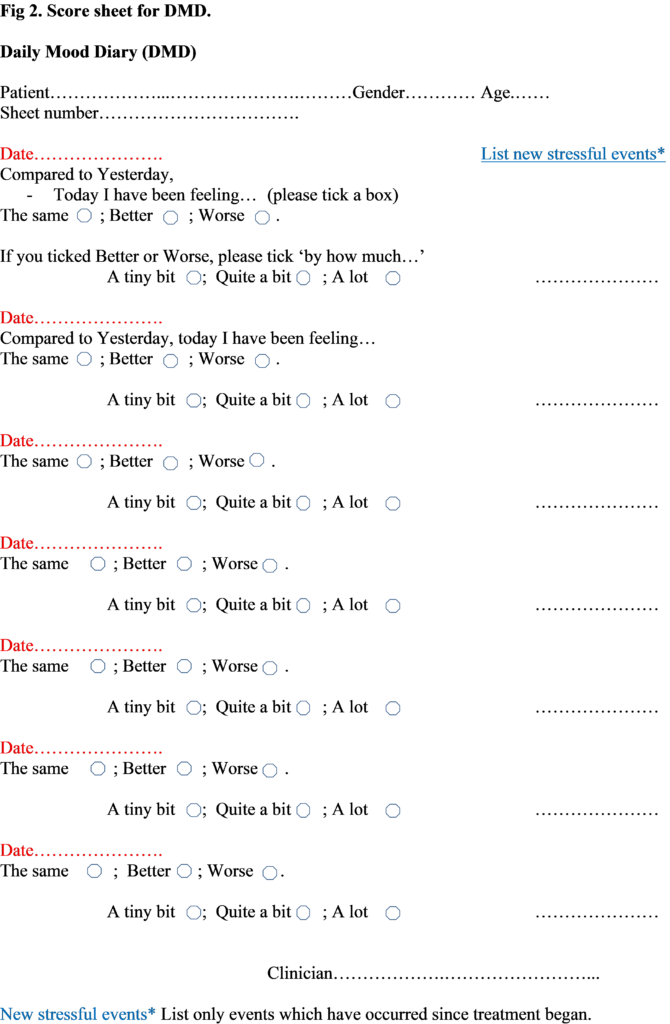
A version of the DMD score sheet is available at the end of this paper (Fig. 2). Interested individuals are invited to make copies and explore whether accurate progressive totals can be collected. On the right-hand side of the page is a space in which recent (since the commencement of treatment) stressful events can be listed. Other versions of this score sheet provide a dedicated space for listing the days ECT and other special treatments have been developed – however, these are not completely necessary – the current version of the score sheet can be easily modified by hand.
The attached MDM score sheet allows 7 days to be recorded. As mentioned, many treatments of acute major depressive disorder (MDD) may take a month to induce remission. In such cases, the attached score sheet is photocopied as necessary.
Transcranial magnetic stimulation (TMS) treatment of acute MDD consists of 20 daily treatments. Patients who have responded to this acute treatment may subsequently receive TMS maintenance courses – five treatments over 5 days, separated by periods of four or more weeks (depending on clinical progress). Should patients have relapsed by the time they return for a scheduled maintenance course, it is possible the 5 treatments will be sufficient to produce remission.
A Case
We present a case of response to a 5-day course of TMS. The patient gave permission for the use of this material and all identifying data has been removed. When the patient returned for 5 days of maintenance, he/she was found to have relapsed on both the 6-item Hamilton Depression Rating Scale (HAMD6), and the Clinical Global Impression – Severity scale (CGI-S). After 4 days of treatment, repeat testing showed that both scales indicated remission had been restored.
Fig. 1 – a case example of DMD
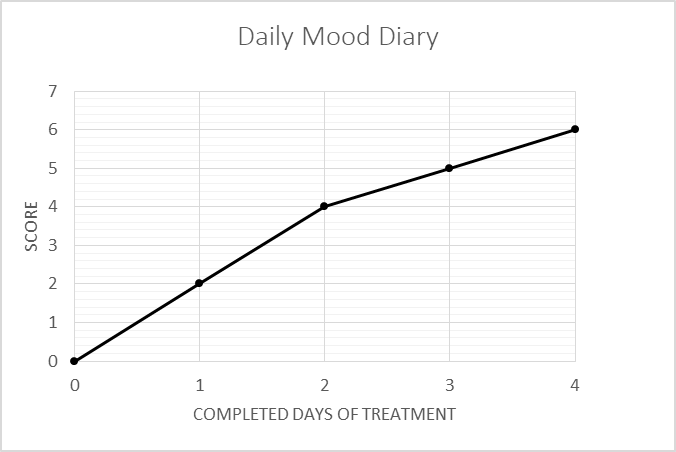
Thus, while the scores of the HAMD6 and the CGI-S fell, the score of the DMD rose. As shown in Fig. 1, at the end of the first day the patients reported feeling ‘Quite a bit’ better (scored 2 points) and this was repeated on the second day. The patient felt ‘A tiny bit’ better after the 3rd and 4th days, giving a rise in score from 0 to 6.
This is suggestive but does not prove the utility of the DMD. We are currently conducting a systematic study to examine this question more closely.