A six-item subjective depression scale is a suitable companion for the six-item Hamilton Depression Rating Scale.
Saxby Pridmore 1, Said Shahtahmasebi2, Yvonne Turnier-Shea 3, Marzena Rybak 3, Rene Morey 3, Ahmed Naguy 4
1Discipline of Psychiatry, University of Tasmania, Hobart, Tasmania, Australia; 2The Good Life Research Centre Trust, New Zealand; 3TMS Unit, Saint Helens Private Hospital, Hobart, Tasmania, Australia; 4Kuwait Centre for Mental Health, Shuwaikh, State of Kuwait.
Correspondance: Prof S Pridmore, email: s.pridmore@utas.edu.au
Received: 20/7/2022; Revised: 25/8/2022; Accepted: 14/9/2022
Key words: Major depressive disorder; Depression rating scales; Hamilton depression rating scale; Subjective depression; Subjective mood.
[citation: Pridmore, Saxby; Shahtahmasebi, Said; Turnier-Shea, Yvonne; Rybak, Marzan; Morey, Rene; Naguy, Ahmed (2022). A six-item subjective depression scale is a suitable companion for the six-item Hamilton Depression Rating Scale. DHH, 9(1):http://www.journalofhealth.co.nz/?page_id=2788].
ABSTRACT
Objective: Major depressive disorder (MDD) is better described when both objective and subjective assessments are acquired. We developed a six-item subjective depression scale (SDS6) to accompany the classic objective six-item Hamilton Depression Rating Scale (HAMD6) as an adjuvant. Method: Items were adopted from the HAMD6, and anchor points were placed either side of ascending numbers in boxes – subjects indicated their experience by ticking appropriate box. Data was collected in a transcranial magnetic stimulation (TMS) unit treating major depressive disorder (MDD) in adults, using naturalistic, quality assurance studies, in which pre- and post-treatment HAMD6 and SDS6 scores were routinely collected in two streams (acute and maintenance treatment). The two scales were correlated using the Spearman rank correlation approach, as the two scales (although numerical) were obtained by qualitative rather than quantitative ratings. Results: 61 patients came from two streams and the total number of pairs for correlation was 188. The Spearman rank correlation coefficient between the two scales is 0.76 (ci 0.69 to 0.83), which is ‘strong’. Conclusion: The SDS6 scores show a strong correlation with the HAMD6 scores, indicating the former subjective tool is a valid measure of the core aspects measured by the latter objective tool. Thus, these tools are useful companions.
Introduction
Major depressive disorder (MDD) and other mood disorders are better understood when both objective and subjective aspects are quantified. The 17-item Hamilton Depression Rating Scale is a classic objective tool. Our group uses the 6-item version (HAMD6) [1] which is time efficient, valid, reliable, and superior to the longer forms in sensitivity [2] scalability and change discrimination [3].
To measure the subjective patient experience, we previously [4] developed a 6-item visual analogue scales (VAS6) based on the HAMD6 items. We assembled these anchor points: ‘Not depressed-Most depressed possible’, ‘No activities give pleasure-Activities give normal pleasure’, ‘No physical health concerns-Extreme physical health concerns’, ‘No guilt feelings-Extreme guilt feelings’, and ‘Not anxious-Most anxious possible’. The final HAMD6 item deals with psychomotor ‘retardation’ which is determined by clinician observation. To approximate this item, we devised a question touching on the experience of concentration difficulties, with the anchor points – ‘Major concentration problems-No concentration problems’. We demonstrated the VAS6 was a valid measure of core aspects of depression and a legitimate companion for the HAMD6 [4].
The VAS6 is straight 10 cm lines with an anchor point at either end. However, some depressed individuals (severe MDD frequently manifests cognitive difficulties) found this tool lacked guiding information and they were uncertain about which direction indicated increase/decrease of particular subjective experiences. Further, data collection was precarious. The VAS6 was reproduced on paper, a ruler had to be found and held on the page, and when the image was reproduced by different processes (printed/photocopied), the length of the line could vary by up to 1 cm, meaning mathematical calculations were necessary to standardize the results of subsequent batches. Accordingly, we developed a replacement tool, the SDS6 scale.
Method
The six-item subjective depression scale (SDS6) employs the items of the HAMD6 and the anchor points of the VAS6 [4]. Unlike VAS6 the SDS6 is a discrete measure where respondents will choose or tick a box as appropriate.
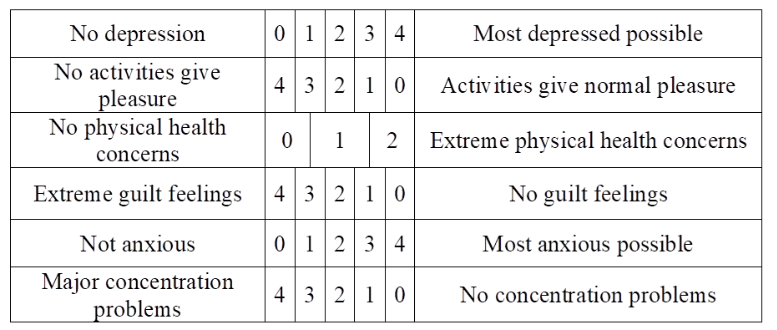
As shown in Table 1, the boxes were orientated such that for the first, third and fifth items the numbers ascend moving to the right, and for the second, fourth and sixth items, the numbers ascend moving to the left. For each item, increasing symptom severity was matched with increasing numerals. The range of the rating options is as they appear in the HAMD6: 0-4 for the first, second, fourth, fifth and sixth items, and 0-2 for the third item [5] (see Table 1).
Table 1. The SDS6: composed of items from HAMD6 with anchor points from the VAS6. Features alternation in the direction of increase in magnitude of response options.
It is postulated that if SDS6 is related to HAMD6 then the former may be a valuable companion for HAMD6 in clinical or non-clinical settings to be used for assessing patients or as a guide. The aim of this study was to explore the relationship, if any, between SDS6 and HAMD6.
Data
A secondary dataset was used for this exploratory study. Data came from quality assurance outcome activities in a transcranial magnetic stimulation (TMS) unit in a private psychiatric hospital, which serves only adults, where pre- and post-treatment responses are routinely collected. The Melbourne Clinic Research Ethics Committee approved the project. Participants were in-patients with MDD and all signed approval for their anonymised data to be pooled and used in institutional clinical assessments.
Data were available from two streams – acute and maintenance treatment. Acute TMS is provided to people with acute (relapsed) MDD with the intention/hope of inducing a remission: 20 treatments are provided on business days over 4 weeks. Maintenance TMS [6] is provided to people with chronic relapsing MDD with the intention/hope of prolonging remission. Five treatments are provided over 2.5-5 days and repeated at monthly or greater intervals. Data on SDS6 was collected as part of this process, from both acute and maintenance TMS courses. We placed the results of these two streams in a single group.
The dataset consists of 61 patients coming from two groups: maintenance (n=36), and acute (n=25). In the maintenance group, some patients had received more than one course of treatment, so the total number of pairs for the correlation analysis (including pre and post treatment as well as repeated patient measurements) was 188.
Results
The overall average HAMD6 score of 5.18 (sd=2.96) is in the expected range – remission is quantified as <4 and relapse as > 7 [7], and the intermediate numbers of >4 & <7 are termed partial relapse/remission [8].
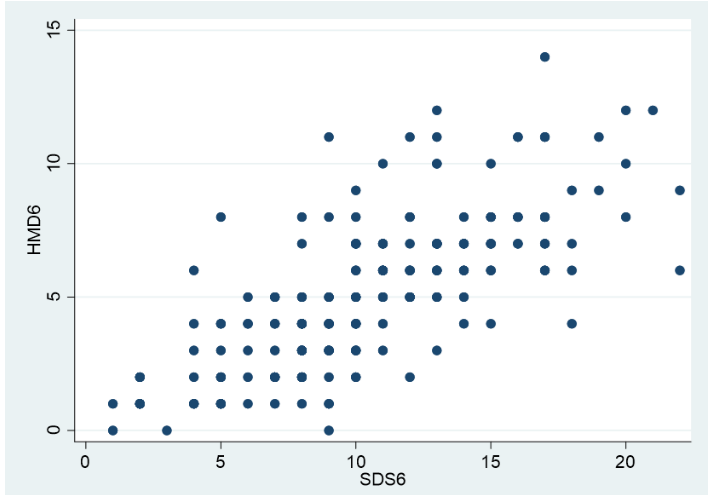
A good way of exploring the relationship between two outcome variables is through a scatter plot. As shown in Fig. 1, a clear positive relationship between the two outcomes can be observed; as one increases so does other. Based on the scatter plot, a correlation coefficient can be calculated, however, there are a number of issues need to be highlighted. A pragmatic approach is to assume that all values, for all intents and purposes, are independent, i.e. that SDS6 and HAMD6 values for pre- or post-treatment, from acute or maintenance stream are from independent respondents.
On the other hand, we may not assume independence because pre- and post-treatment, and acute or maintenance values for HAMD6 and SDS6 are collected for each subject. Therefore, the inclusion of multiple observations or repeated measures for the same individuals will lead to serial correlation which may lead to an over-estimation problem. This is particularly important when calculating standard errors, necessary for providing confidence intervals for the coefficients obtained. For this analysis, we used the Spearman rank correlation technique using bootstrap to correct for bias due to repeated measures.
The bootstrapped Spearman correlation obtained for the total sample analysis was 0.76 (confidence interval 0.69 to 0.83). As the correlation is >0.7, it is described as “strong”. In other words the visual relationship between HAMD6 and SDS6 shown in Fig. 1 is strongly supported by the correlation coefficient.
Fig 1. A scatter plot illustrating the relationship between the total scores of the six-item Hamilton Depression Rating scale (HAMD6) and the six-item Subjective Depression Scale (SDS6).
Discussion
The quantification of mood is a central task of psychiatry. For comprehensive, accurate assessment, quantification of both objective and subjective aspects is recommended.
Earlier, we developed the VAS6 [4] to harvest subjective experience, and found it a credible companion for the HAMD6. However, some patients and staff found completing this test somewhat challenging. As a result SDS6 was developed to iron out the problematic issues. Over the last year patients have consistently reported the SDS6 easy to understand and expeditious to complete. Of those patients who have had experience of both the VAS6 and the SDS6 there is almost unanimous support for the latter tool. Staff also prefer the SDS6 as data extraction.
The HAMD6 is well validated – this study shows the subjective SDS6 is strongly correlated with the HAMD6, indicating the SDS6 may be a suitable complimentary tool to be paired with this classic objective scale. Data was drawn from a real-world setting, and reflects the outcome of our routine clinical practice.
Our aim was to evaluate the SDS6 as a companion for the HAMD6: we found an overall “strong” correlation, or relationship between these two measures. This indicates the subjective SDS6 is an appropriate companion tool for the HAMD6. Had we further resources, we would have examined the correlations of the six items separately. We previously examined the correlations of the VAS6 and the HAMD6 [4]. The Spearman correlation for the total scores (using a different methodology) was moderate-strong.
It is of interest, the average SDS6 score (10.52, sd=4.59) was double the HAMD6 score. One explanation could be that SDS6 is a measure of how the respondents felt at the time of the survey whilst HAMD6 is a measure what the clinicians believe the respondents felt. Therefore, assuming the latter to represent a more objective (true) value then SDS6 is the true value plus some error. This phenomenon is clearly demonstrated in Fig. 1, i.e. the relationship between the two variables is in the same direction but scatter, as opposed to a narrow spread and along a straight line. Nevertheless, the evidence suggest that SDS6 could well be a subjective mood tool to compliment the objective HAMD6.
One of the limitation of this kind of study is that subjective measures (such as self-assessment or self-reporting) invariably carry errors which may explain discrepancies in the relationship between the objective HAMD6 and SDS6. Nevertheless, such measures are based on the subject’s own assessment and reflect how they are feeling rather than how they should be feeling. Therefore, the strong correlation between the two measures, warrant using the subjective SDS6 to compliment clinical assessments. However an advantage of using such data is that the data reflect real life practical experiences.
We recommend that future research concentrate on applying SDS6 with a much larger sample within a well-designed study to be used in general practice as a guide.
Conclusion
The SDS6 total score correlates strongly with the HAMD6 total score, identifying the subjective SDS6 as a suitable companion to the HAMD6, which may now be adopted by others. In routine clinical work the SDS6 has been welcomed as by patients and staff alike.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflict of Interest: The authors declare no conflicts of interest.
Acknowledgements: Ricardo Maldonado, Power Stats, West Ryde NSW, Australia, for his professional statistical services.
References:
- Bech P, Allerup P, Gram L, et al. (1981) The Hamilton Depression Scale. Acta Psychiatr Scand 63(3): 290-299. doi: 10.1111/j.1600-0447.1981.tb00676.x.
- O’Sullivan R, Fava M, Agustin C, et al. (1997) Sensitivity of the six-item Hamilton Depression Rating Scale. Acta Psychiatr Scand 95(5):379-384. DOI: 1111/j.1600-0447.1997.tb09649.x
- Kyle P, Lemming O, Timmerby N, et al. (2016) The validity of the different versions of the Hamilton Depression scale in separating remission rates of placebo and antidepressants in clinical trials of major depression. J Clin Psychopharmacol 36(5): 453-456. DOI: 1097/JCP.0000000000000557
- May T, Pridmore S. (2020) A visual analogue scale companion for the six-item Hamilton Depression Rating Scale, Australian Psychologist 55(1): 3-9. https://doi.org/10.1111/ap.12427
- Pridmore S, Naguy A, Pridmore W, et al. (2021) A new six-item subjective depression scale (SDS-6). Dynamics of Human Health 8(4). http://www.journalofhealth.co.nz/wp-content/uploads/2021/12/DHH_Depression_Saxby.pdf
- Fitzgerald P, Grace N, Hoy K, Bailey M, Daskalakis Z. (2013) An open label trial of clustered maintenance rTMS for patients with refractory depression. Brain Stimul 6(3): 292–297. http://doi: 10.1016/j.brs.2012.05.003.
- Bech P, Lunde M, Bech-Andersen G, et al. (2007) Psychiatric outcome studies (POS): Does treatment help the patients? A Popperian approach to research in clinical psychiatry. Nord J Psychiatry 61(Suppl 46): 4-34. http://doi: 10.1080/08039480601151238.
- Rush A, Kraemer H, Sackheim H, et al. (2006) Report by the ACNP Taskforce on response and remission in major depressive disorder. Neuropsychopharmacology 31(9): 1841-1853. http://doi: 10.1038/sj.npp.1301131.